Snakebite Crisis in India is a Silent Public Health Emergency, Claiming Tens of Thousands Annually

On a humid evening in rural eastern India, a farmer walking home from his fields feels a sudden sting on his ankle. By the time his family arranges transport to the nearest hospital that is hours away, the venom has already done its worst. Stories like this play out on daily bases across India, which bears the heaviest global burden of snakebite deaths. A largely preventable public health crisis that continues to receive limited political and medical attention.
India records an estimated 50,000 to 58,000 snakebite deaths every year. Roughly half of all global fatalities. A landmark 20-year study covering 2000 to 2019 put the average annual death toll at around 58,000, though experts believe the real number is higher due to widespread under-reporting. Snakebites are most common in rural, agricultural regions, particularly in central and eastern states, where farm workers, women collecting firewood, and people from poor tribal communities are most exposed.
Despite the scale of the problem, snakebite envenoming remains a neglected disease. The World Health Organization classifies it as a “highest priority neglected tropical disease”, noting that it overwhelmingly affects low-income rural populations. In India, the victims are often those with the least access to healthcare and the weakest political voice.


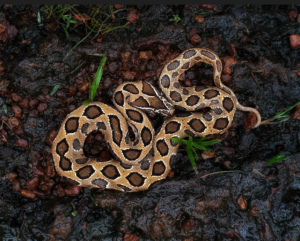
Most fatal bites are attributed to the so-called ‘Big Four’ snakes, the Indian cobra, common krait, Russell’s viper and saw-scaled viper. India’s public health system relies on antivenom developed to counter these species. But the country is home to dozens of venomous snakes, many of which are region-specific. Studies have shown that existing antivenom can be ineffective against bites from lesser-known species, leading to poor treatment outcomes and prolonged illness.
Even when antivenom is available, reaching it in time is a major challenge. Hospitals equipped to handle snakebite cases are often far from villages, connected by poor roads and limited transport. Ambulance services are scarce, and families frequently rely on motorcycles or private vehicles, losing critical hours. A recent report found that 99% of healthcare workers face obstacles in administering antivenom, including shortages, lack of cold-chain storage, and insufficient training.
 At the grassroots level, mistrust of the formal health system and innate beliefs also play a role. Many victims first turn to faith healers or traditional remedies, delaying hospital treatment. By the time they arrive at a medical facility, complications such as severe tissue damage, organ failure, or permanent disability may have set in. Survivors often face amputations or lifelong mobility issues, pushing already poor households deeper into poverty.
At the grassroots level, mistrust of the formal health system and innate beliefs also play a role. Many victims first turn to faith healers or traditional remedies, delaying hospital treatment. By the time they arrive at a medical facility, complications such as severe tissue damage, organ failure, or permanent disability may have set in. Survivors often face amputations or lifelong mobility issues, pushing already poor households deeper into poverty.
Government attention to the crisis has grown, but unevenly. In 2024, India launched the National Action Plan for Prevention and Control of Snakebite Envenoming (NAPSE), aiming to cut snakebite deaths by half by 2030. The plan focuses on improving surveillance, ensuring antivenom availability, training healthcare workers and raising public awareness. However, implementation has been inconsistent across states, with snakebite still widely viewed as a “poor person’s problem”.
Some states have taken stronger steps. Karnataka, for example, has made snakebites a notifiable disease, requiring all cases to be officially reported. Public health experts say such measures are crucial to understanding the true scale of the crisis and directing resources where they are most needed.



Doctors, researchers and community workers argue that technical solutions alone are not enough. What is needed is sustained political will, such as investment in rural healthcare, region-specific antivenom research, reliable transport systems and community sensitization that encourages early hospital treatment. As one public health expert put it, snakebite deaths are not inevitable acts of nature, but a reflection of inequality within a nation, caused by lack of political will to enforce government social-security structure for her citizens.
Until India treats snakebite envenoming as the national emergency that it is, tens of thousands of preventable deaths will continue to occur quietly each year, devastating families and communities.








